Global health pioneer earns university’s top academic title
Rice University’s Rebecca Richards-Kortum, a pioneer in both bioengineering and global health, has become the first woman and the youngest Rice faculty member to earn the rank of University Professor — Rice’s highest academic title.
The promotion is the latest in a string of high-profile honors for Richards-Kortum this year. In April, she was elected to both the American Academy of Arts and Sciences and to the National Academy of Sciences — the latter earning her the rare distinction of dual memberships in the National Academy. (She was elected to the National Academy of Engineering in 2008). In June, she received a presidential appointment to the White House committee that evaluates nominees for the National Medal of Science.
Richards-Kortum’s appointment as the Malcolm Gillis University Professor and professor of bioengineering and of electrical and computer engineering became effective July 1. At age 50, she becomes only the seventh Rice faculty member to hold the rank of University Professor and the first to earn the title since mathematician Richard Tapia in 2005.
The title of “University Professor” is an appointment-at-large that enables the faculty member to teach in any academic department and share expertise broadly across disciplines to foster greater intellectual pursuits at Rice.
Richards-Kortum joined Rice’s faculty in 2005, and just a year later she and Bioengineering’s Maria Oden co-founded one of the most popular and transformative educational programs in Rice’s history, the award-winning, hands-on engineering education program Beyond Traditional Borders. In its first five years, the program attracted more than 10 percent of Rice’s undergraduate students, including many non-engineering students. The program led Rice to establish a minor in global health, and it helped drive activity at Rice’s award-winning Oshman Engineering Design Kitchen, where students have produced more than 60 low-cost health technologies, including “bubble CPAP,” a low-cost version of the continuous positive airway pressure, or CPAP, systems that are commonly used in developed countries.
Richards-Kortum serves as director of Rice 360°: Institute for Global Health Technologies and of the Rice Institute of Biosciences and Bioengineering. Her laboratory focuses on developing point-of-care diagnostic technologies that are inexpensive and portable for diseases ranging from cancer to malaria. Her work has produced 29 patents, more than 230 research papers, 11 book chapters and the textbook Biomedical Engineering for Global Health.
Rice’s other University Professors include Nobel laureates Robert Curl and the late Richard Smalley, former White House science adviser Neal Lane, former Rice President Malcolm Gillis and the late Ken Kennedy, who was a nationally renowned computer scientist.
Rice News recently caught up with Richards-Kortum after a trip to Africa that included time in Malawi, a country that has hosted Rice undergraduate global-health interns for the past nine years.
—
Rice News: Being made a University Professor is partly a recognition that you have changed Rice in a significant way. Were you thinking, “I’m going to put my mark on this place,” when you arrived in 2005?
Richards-Kortum: No, I definitely didn’t. It was really important to me to make significant contributions to Bioengineering. I came in thinking, “I will change Bioengineering. Hopefully, I’ll make Bioengineering better.”
I didn’t think that I would have the opportunity to work more broadly across campus and to focus so much on the role that technology could play in reducing health disparities. I think that’s been a really amazing and exciting opportunity, to be able to reach more broadly across campus and work with students from engineering, the natural sciences, social sciences, humanities and architecture and to think about how we can collaborate together. Not just come up with ideas that could make a difference, but actually then put those ideas into practice.
I think the trip to Malawi that I just took was really a wonderful opportunity to see the culmination of that because for the first time we have interns from Rice and we have interns from Malawi Polytechnic, and they’re working together. There’s a group working together in Malawi, and there’s another group working together in Houston.
Now we have this bilateral, bicultural, multidisciplinary exchange of students. They’re actually in the field working together to try and come up with solutions, but also to implement solutions and see the work of other technologies that have been previously implemented. That was a pretty nice moment — to see them, to see how important that experience is to them, to gain a better appreciation of what some of these big challenges are and to give them the opportunity to actually experience being part of the solution while they’re still students.
Rice News: It seems that you are driven to try to make the world a better place.
Richards-Kortum: I think, for me personally, it’s hard to separate the perspective of being a mother and thinking about what I hope to accomplish in my career. I think nobody who’s a mother or a father can go to Malawi and visit a nursery there and not feel that this is just so wrong, that the babies there have access to so little of the basic technologies that we just completely take for granted. Hospitals here don’t run out of Tylenol; the power doesn’t go out every day; babies don’t die because they’re cold.
I think being a parent shaped a lot of what I hope I can achieve through my career, but also, more importantly, what I hope the students that I teach can accomplish in their careers.
Rice News: If there was a watershed moment for you, was it that first trip to Malawi?
Richards-Kortum: Oh yeah. Certainly. I taught classes in bioengineering and world health, but it’s very different to go and meet mothers who have children in a hospital that lacks so many basic things and to meet physicians and nurses who have dedicated their whole lives to trying to provide the very best health care that they can in that setting. I came back from the (first) trip in 2005 with a completely transformed view of what was needed and what I hoped I could accomplish through working with faculty and students here.
Rice News: When you came back from that trip, a lot happened in a relatively short amount of time. Is there any one thing that you can point to that allowed that to take place?
Richards-Kortum: I think the thing that made a difference was that we had a belief that students here were capable of solving some of these technology challenges. There were some people who were early believers. Maria Oden was one of the very first. She was teaching our senior design class when I came here, and I talked to her about this idea, and she immediately just joined in and contributed so much to believing in the idea and actually putting it into practice.
When I think back to when we started that 10 years ago, there were a lot of people who just didn’t believe, I think, that it was possible for this to result in improved health care. I think people accepted that this would be a good educational experience, but not necessarily that it could really result in improved health care.
Now, when we travel to Malawi, CPAP is in every government, central and district hospital. If I walk into a hospital and I say, “We’re here to see a CPAP,” people immediately know where it is. They know where to go. They can show us where it is and how it’s being used.
The program has produced a technology that has had a countrywide impact in Malawi and even beyond Malawi. There’s plenty more that’s needed, and we’ve got plenty more in the pipeline behind it, but it definitely started from a belief. It was just working day to day to actually make that happen.
Rice News: Because of how much that first visit affected you, did you know that that kind of experience would be a key part of the educational experience for students?
Richards-Kortum: Yes. We were really fortunate that we wrote this proposal to the Howard Hughes Medical Institute to build what is now the global health technologies minor. We decided we would get design challenges from practicing clinicians in places like Malawi, and we would put student teams together and allow them to go overseas in the summer and put their ideas into practice. The proposal had all of that built in. HHMI believed in that idea, and we were so lucky that they did because those resources allowed us, then, to demonstrate that indeed it was possible to do this as more than something that would benefit the students here.
Rice News: One of the fascinating things about the Design Kitchen and the global health minor is how emotionally vested the students become and how devoted they are to solving these problems. Did you anticipate that?
Richards-Kortum: I came back a different person, so I was pretty sure other people would come back different. I was just reading the student blogs from this year, and there’s one from Renata Wettermann, who is at St. Gabriel’s Hospital. She’s been interested in the issue of morphine dosing. She wrote a blog post where she said, “(When) I learned about this in class, it was this theoretical exercise.” Then she did a home visit with one of the community health workers, and they visited a patient who was dying from advanced HIV and anal cancer.
She wrote about what it was like to see what horrible pain this patient was in and how morphine is what allows us to help people preserve their dignity at the very end of their lives. She’s not going to come back the same from Malawi.
The other thing that we’re doing this year that I think is hugely important, and I’m so happy that we’re finally able to do it, is now we’re teaming Rice students with students from Malawi. What the Rice students have told us this summer is that they have learned so much from working together with the Malawian students and that their expertise is so complementary, and that they’ve been able to be so much more productive.
We have one student who was there last year, when they weren’t working with Malawian students, and she’s there again this year. She said, “We’re getting so much more done as a team together and building these relationships.”
Rice News: When did you decide you wanted to be a professor?
Richards-Kortum: I debated a lot at the end of grad school. I applied for faculty and industry jobs, and I really went back and forth a lot. In the end, I decided that teaching was very important to me. I felt like I could do the research that I wanted either in a university or in a company, but teaching really was fundamentally important to me, and so that’s why I ended up where I did.
Rice News: What was your research goal at the outset of your career?
Richards-Kortum: I was really interested in cancer screening and early diagnosis, and so in grad school, I worked on technologies that were related both to diagnosis and treatment of heart disease and also cancer. I was really fascinated by how we could develop imaging systems that would help physicians identify cancers at an earlier and more treatable stage. That was really the focus of my research. It had a completely developed-world focus at that time.
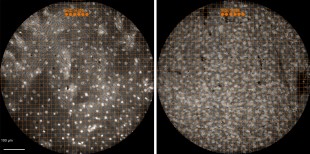
In these images from Rice’s high-resolution microendoscope, the white spots are cell nuclei, which are irregularly shaped and enlarged in cancerous tumors (right) as compared with healthy tissue (left). Credit: Richards-Kortum Lab/Rice University
Rice News: We recently had a story about the results from one of the first clinical studies of your high-resolution microendoscope. Is that one thing you can check off your list?
Richards-Kortum: I think it was really nice to see the results of that study. I feel like we made really major progress toward having something that can make a significant difference there. There’s still a lot to be done to translate it, to get it so that it’s out and being used as part of patient care. But I think we have a technology that really addresses a significant part of the need.
Rice News: I know it’s hard to look into the future, but imagine it’s 10 years from now. What do you hope to have checked off your list then?
Richards-Kortum: One thing I really hope to do is develop what we call the “Nursery of the Future,” which is a complete set of technologies that provides for all of the basic needs for newborn care at district-level hospitals. Our goal is to do this for a total cost of $5,000 to $10,000 for a hospital that serves a community of 250,000 people. I think it’s possible. CPAP is really the first piece of that, but together with Maria and the team, we have a whole pipeline of technologies that are at various stages of development. I think in a five- to 10-year time frame it is possible to develop those and to implement them in the same way that we’ve implemented CPAP.
Rice News: Can you describe how it feels when you walk into a hospital in Malawi and see a CPAP and know that it was your students who helped create it?
Richards-Kortum: It’s interesting. It goes one of two ways. Maria and I have visited hospitals where it’s making a difference. Babies are alive that probably would not have survived had it not been there. And we got to see those babies. Who could ask for a better moment?
Then, you walk into other hospitals, and it’s just sitting on a shelf. The challenges associated with effectively putting new technology into a hospital are one of the things I totally underestimated. As an engineer, you think that if you make something, and it works, your job is done.
But your job has just begun. Because there are so many challenges that make it difficult to have that technology be properly used and well-used over time. We’ve got a lot of work to do, as a team, to make sure the technologies are used well.
Rice News: Is it just a matter of training?
Richards-Kortum: It’s more complicated than that. Nurses do need to be trained to use CPAP, but what we didn’t realize is that there are other issues. At some hospitals, nurses get rotated off the pediatrics ward every six months. Just because everyone was trained in January, that doesn’t mean they will still be there in July. What do you do in July? Do you go back? How do you afford to keep doing that?
What we’re doing now is going into the nursing schools and implementing training there. The other thing that we didn’t think about is, let’s say a baby is in respiratory distress and they’re on CPAP. If they’re cold because it’s too cold in the nursery, CPAP is not enough. It’s not as effective. That’s why we’re now taking a more comprehensive approach.
Rice News: What else would you like to accomplish at Rice?
Richards-Kortum: One thing I’ve been thinking about lately is a “gap year” program. It’s just an idea right now, but Rice 360° has been hiring a lot of postbaccalaureate students like Jocelyn Brown, Mary-Kate Quinn, Alexa Juarez and others, and they have contributed so much to getting promising technologies into the clinical pipeline.
Normally, when people take a gap year, they take it in between high school and college, but what if students took it after they got their undergraduate degree? They could take a year or two and really focus on using their skills to solve a problem that addresses health inequity.
Students, at that point in their career, have enough disciplinary knowledge that they can make really meaningful contributions if their energy is focused on a particular problem. We’ve seen that happen, and I’ve been thinking about ways to build upon that.
Rice News: As a University Professor, you can teach in any department. Have you thought about a new class you’d like to teach?
Richards-Kortum: No, but I have been thinking about how to mentor students to think in a more problem-focused way. In a sense, that’s not what we train Ph.D. students to do. Innovation tends to be the focus there, rather than thinking about how things are put into practice. I’ve been thinking about how to approach problems so that there’s a mix of innovation and putting things into practice.
For example, a student may be working toward a technology that is truly innovative, but it has a 20-year horizon before it’s going to be developed and through the regulatory process. That may sound like a long time, but 17 years is the average time to get something from conception to implementation.
That’s a long time to wait in a setting where babies are dying because they’re cold. I’m really interested in thinking about how to blend short-term solutions and the more innovative thinking that might also have a longer horizon.





Leave a Reply